Phone:
+6011-56331685
Email Address:
theneurofit@gmail.com

In our last post, we introduced sarcopenia, the “silent muscle thief,” and talked about why this age-related loss of muscle mass, strength, and function is so important to recognize. Now, let’s dive into how sarcopenia is diagnosed and assessed, with a special focus on the crucial role physiotherapy plays in this process.
Despite its significant impact on health, sarcopenia often goes unrecognized. One reason for this has been the historical lack of a single, universally accepted definition. Various international groups, like the European Working Group on Sarcopenia in Older People (EWGSOP/EWGSOP2) and the Asian Working Group for Sarcopenia (AWGS/AWGS2), have proposed different frameworks to identify the condition. The good news is these groups are working towards a global consensus, aiming for clearer guidelines.
From a physiotherapy perspective, the updated EWGSOP2 definition is especially relevant. It emphasizes a practical, step-by-step approach summarized by the F-A-C-S algorithm: Find-Assess-Confirm-Severity.
• Probable Sarcopenia: Identified primarily by low muscle strength.
• Confirmed Sarcopenia: Diagnosed when there’s low muscle strength PLUS low muscle quantity/quality.
• Severe Sarcopenia: Present when all three criteria are met: low muscle strength, low muscle quantity/quality, AND poor physical performance.
This phased approach helps us pinpoint the severity of muscle loss and tailor interventions accordingly.
Physiotherapists are on the front lines of assessing muscle health and function. We use a range of practical, evidence-based tools recommended by EWGSOP2 to identify, confirm, and determine the severity of sarcopenia.
1. Case Finding/Screening: Initial Clues
These tools help us quickly identify individuals who might be at risk, prompting a more detailed assessment.
• SARC-F questionnaire: This is a simple, 5-item self-reported questionnaire. It asks about difficulties with everyday activities like lifting, walking, rising from a chair, climbing stairs, and any falls. It’s easy to use in a clinic or even at home.
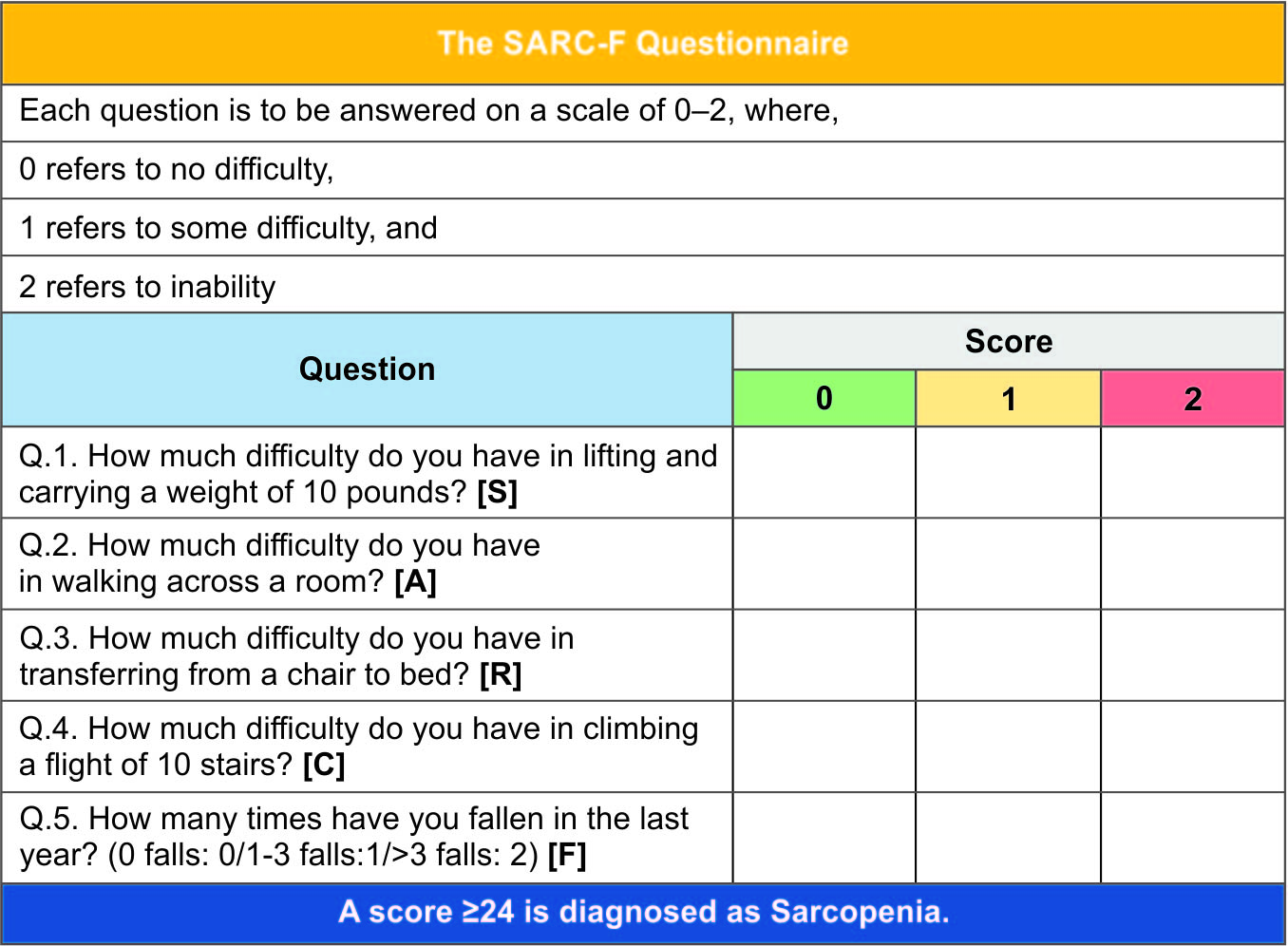
(SARC-F Questionnaire From Journal of The Association of Physicians of India)
• Ishii screening tool: This tool estimates sarcopenia probability using easily accessible measurements like age, grip strength, and calf circumference.
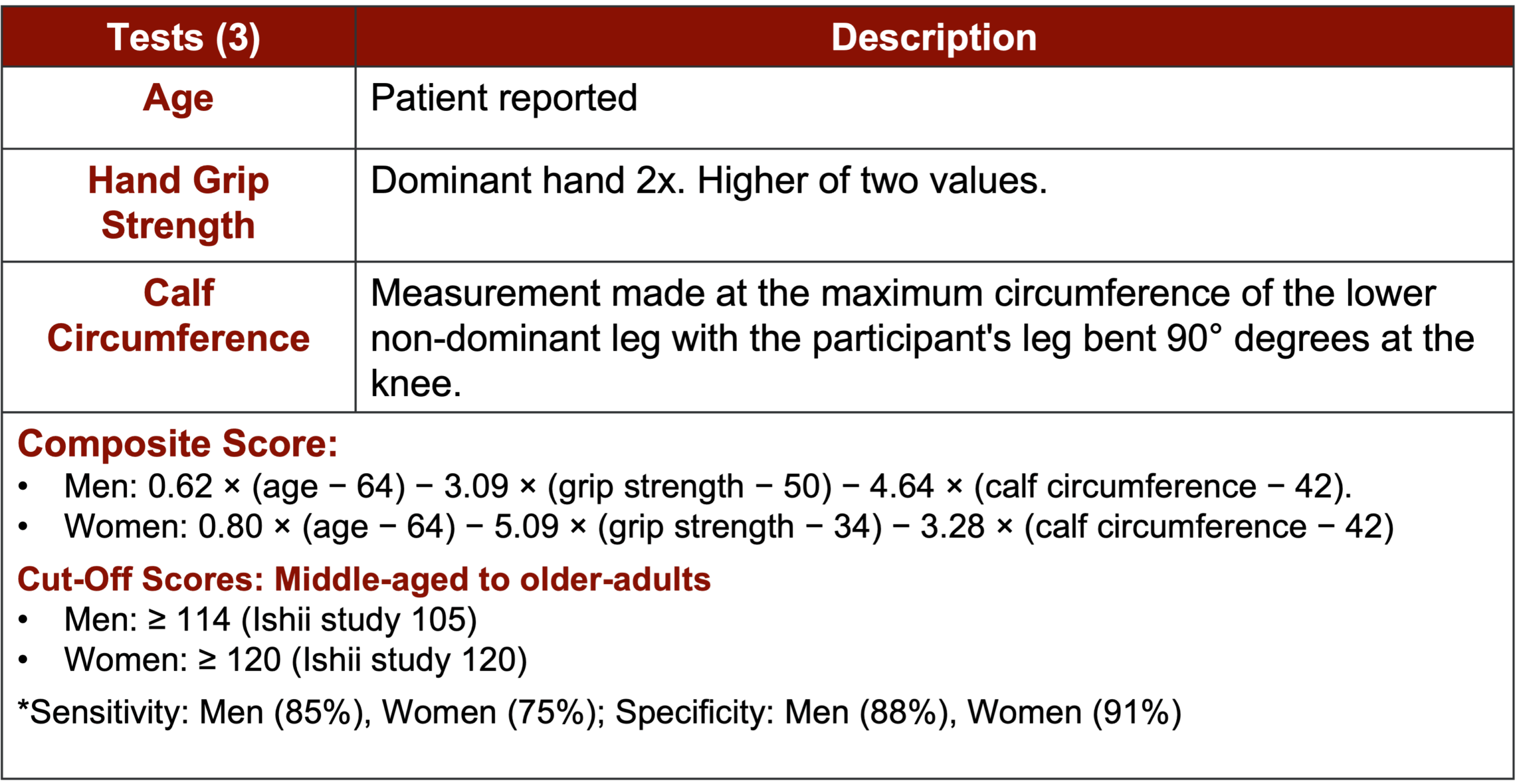
(Ishii Screening tool from Physicaltherapy.com)
2. Muscle Strength: A Key Indicator
Low muscle strength is the cornerstone of a sarcopenia diagnosis. Physiotherapists directly measure this to understand your current capacity.
• Handgrip Strength (HGS): This is a simple, inexpensive, and incredibly robust indicator of overall physical mobility and strength. You just squeeze a device called a dynamometer. The EWGSOP2 recommends thresholds of less than 27 kg for men and less than 16 kg for women as indicators of low grip strength.

(Dynamometer hand grip test Image From OPC Health)
• Chair Stand Test (CS): Also known as the 5-times sit-to-stand test, this measures the time it takes you to stand up and sit down five times from a chair without using your arms. It’s a fantastic, convenient measure of lower body strength and power. A time greater than 13 seconds suggests a higher risk of sarcopenia.
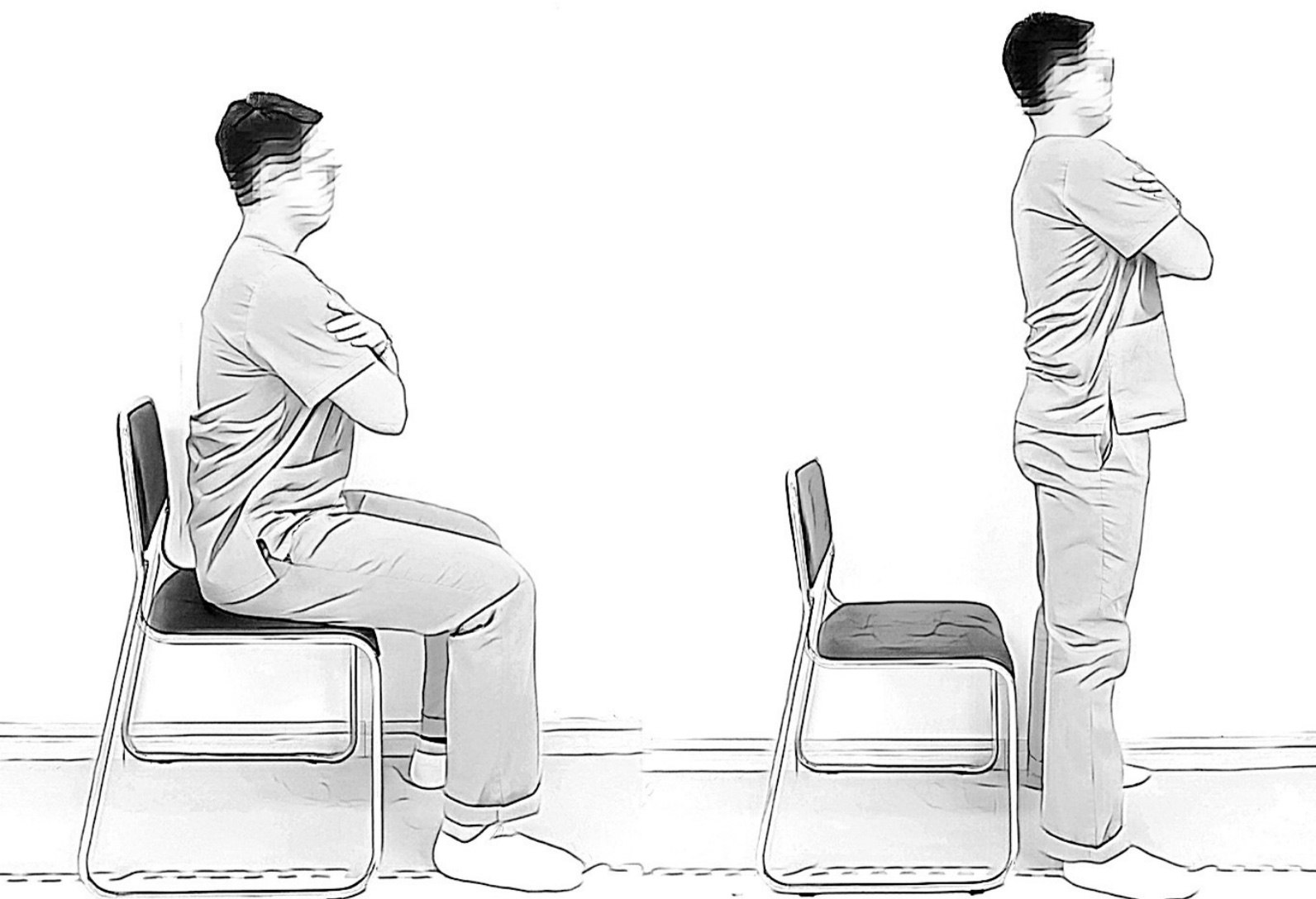
(Image From Annals of Geriatric Medicine and Research)
3. Muscle Quantity/Quality: The Deeper Dive
While some of these methods are typically performed in a hospital or specialized facility, understanding them helps complete the diagnostic picture. Physiotherapists use the results of these tests to inform your treatment plan.
• Dual-energy X-ray Absorptiometry (DXA): Often considered a “gold standard,” DXA scans provide precise, non-invasive measurements of muscle mass, particularly in your arms and legs (appendicular skeletal muscle mass).

(DXA Image From Diabecare Diabetes and Endocrine Clinic)
• Bioelectrical Impedance Analysis (BIA): This is a more affordable, portable, and widely available method. It estimates muscle mass based on how electrical currents pass through your body. While practical, factors like hydration and ethnicity can influence its accuracy.
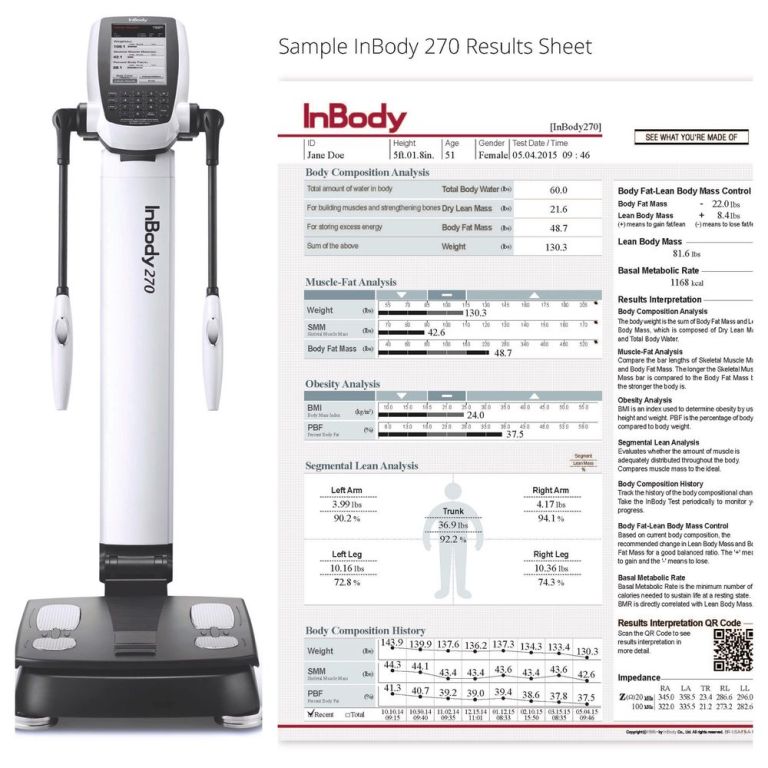
(BIA image from InBody)
4. Physical Performance: Real-World Function
This is where physiotherapy truly shines. We directly assess your functional abilities, which is critical for determining the severity of sarcopenia and its impact on your daily life.
• Gait Speed: This is a quick, safe, and highly reliable test where we measure how fast you walk a short distance (e.g., 4 meters). A speed of 0.8 meters per second or less is a strong indicator of severe sarcopenia and increased risk of adverse outcomes.
• Timed Up and Go (TUG) test: This test measures the time it takes to stand up from a chair, walk 3 meters, turn around, walk back, and sit down again. A time greater than 20 seconds strongly predicts poor physical function and higher fall risk.
Understanding your muscle health is the first step towards taking control. An accurate diagnosis of sarcopenia allows your healthcare team
• Create a personalized treatment plan: Tailored exercises and strategies to address your specific deficits in strength, mass, and function.
• Prevent further decline: Early intervention can significantly slow or even reverse muscle loss.
• Reduce risk of falls and injuries: By improving your balance and strength.
• Improve your overall quality of life: Enabling you to maintain independence and enjoy daily activities.
If you’re concerned about your strength, mobility, or think you might be at risk for sarcopenia, don’t wait. A comprehensive assessment from a physiotherapist can provide valuable insights and set you on the path to a stronger, healthier future.