Phone:
+6011-56331685
Email Address:
theneurofit@gmail.com

Not all strokes are the same. Strokes are complex medical events with varying outcomes, influenced by several factors, including the type, location, and severity of the stroke, as well as the time that has elapsed before treatment. These factors significantly impact the prognosis, recovery process, and rehabilitation strategies. By understanding these elements, we can better approach stroke recovery with more tailored and effective treatments.
1. Ischemic Stroke
• Causes: Ischemic strokes occur when a blood clot blocks or narrows an artery, disrupting blood flow to a part of the brain.
• Specific Locations:
◦ Middle Cerebral Artery (MCA) Stroke: The most common type, affecting areas that control speech, movement, and sensation on the opposite side of the body.
◦ Anterior Cerebral Artery (ACA) Stroke: Affects the front of the brain, leading to leg weakness, mental changes, and sometimes paralysis on one side of the body.
◦ Posterior Cerebral Artery (PCA) Stroke: Can cause visual disturbances, memory loss, and sensory problems.
• Prognosis: A better prognosis is possible if treated promptly, with rehabilitation playing a crucial role in long-term recovery. The extent of brain damage and the stroke’s location influence recovery potential.
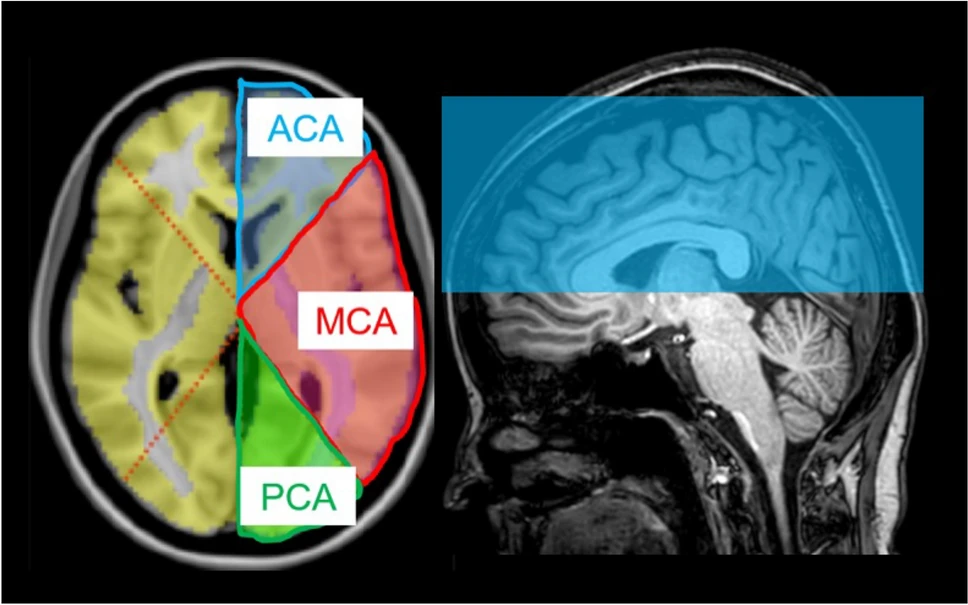
Image Source: Kikuchi, K., Togao, O., Yamashita, K. et al. Brain volume measured by synthetic magnetic resonance imaging in adult moyamoya disease correlates with cerebral blood flow and brain function. Sci Rep 14, 5468 (2024). https://doi.org/10.1038/s41598-024-56210-2
2. Hemorrhagic Stroke
• Causes: Hemorrhagic strokes are caused by the rupture of blood vessels in or around the brain, leading to bleeding and increased pressure on the brain tissue.
• Specific Locations:
◦ Intracerebral Hemorrhage (ICH): Bleeding within the brain tissue itself, often caused by high blood pressure or trauma.
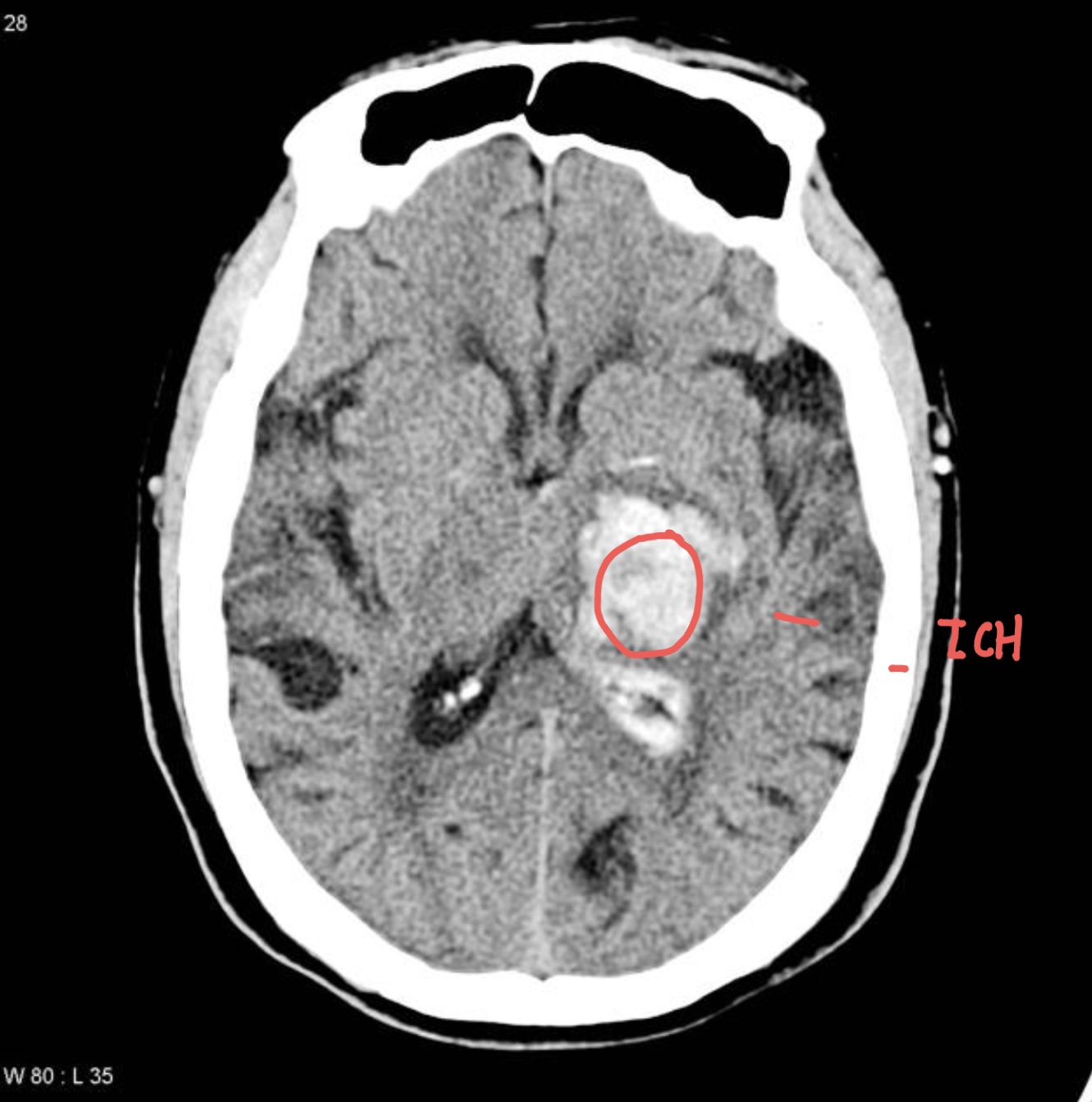
Image Source: Radiopaedia
◦ Subarachnoid Hemorrhage (SAH): Bleeding in the space surrounding the brain, commonly caused by aneurysms.
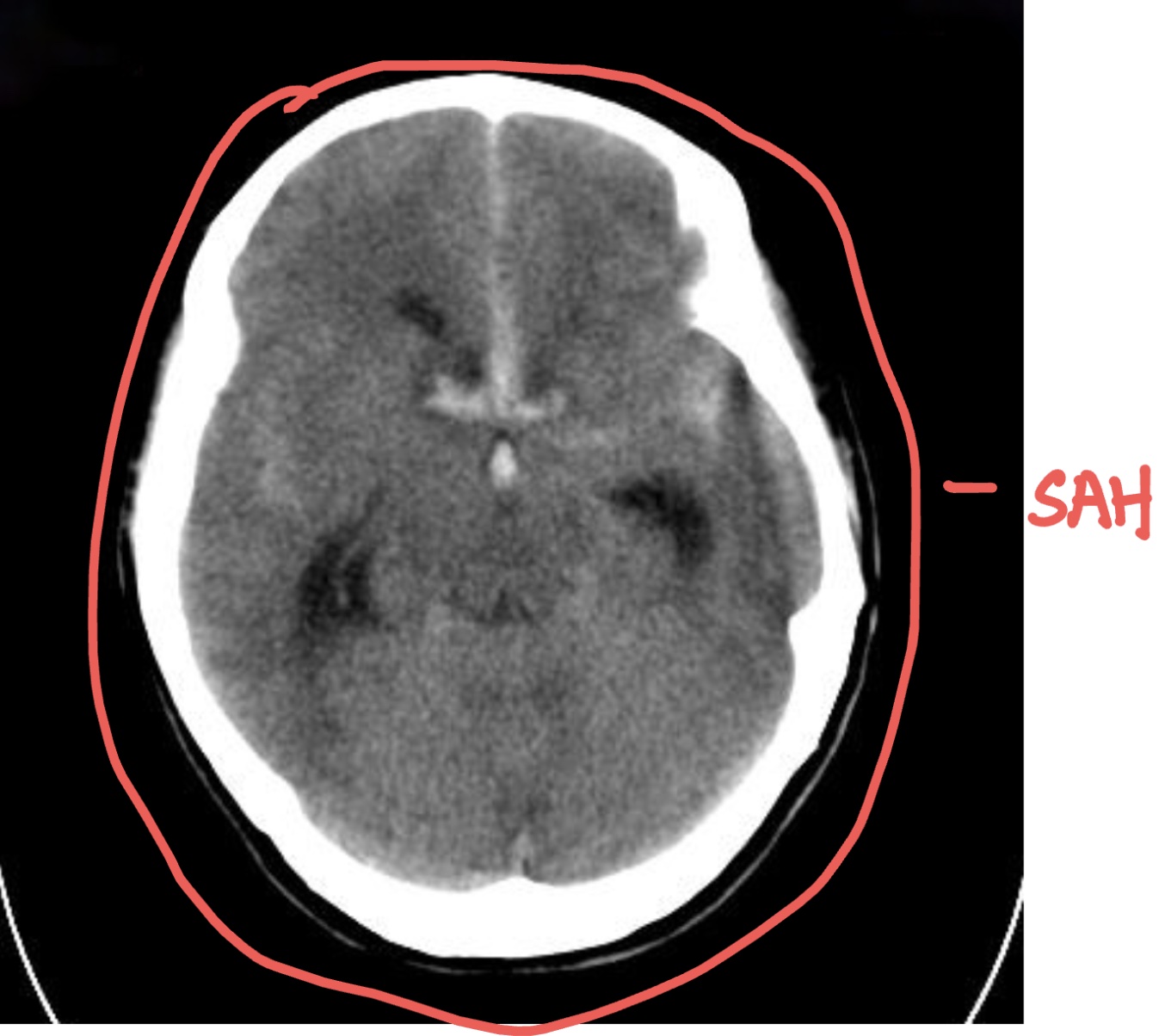
Image Source: Radiopaedia
• Prognosis: Generally worse than ischemic strokes due to the potential for more extensive brain damage. The severity and location of the hemorrhage are critical in determining recovery the outcome of recovery.
3. Transient Ischemic Attack (TIA)
• Causes: Often referred to as a “mini-stroke,” a TIA is caused by a temporary blockage in blood flow to the brain. It mimics stroke symptoms but does not cause permanent damage.
• Prognosis: Good if preventive measures are taken; however, TIAs are strong indicators of a higher risk of a future stroke, and immediate medical attention is critical.
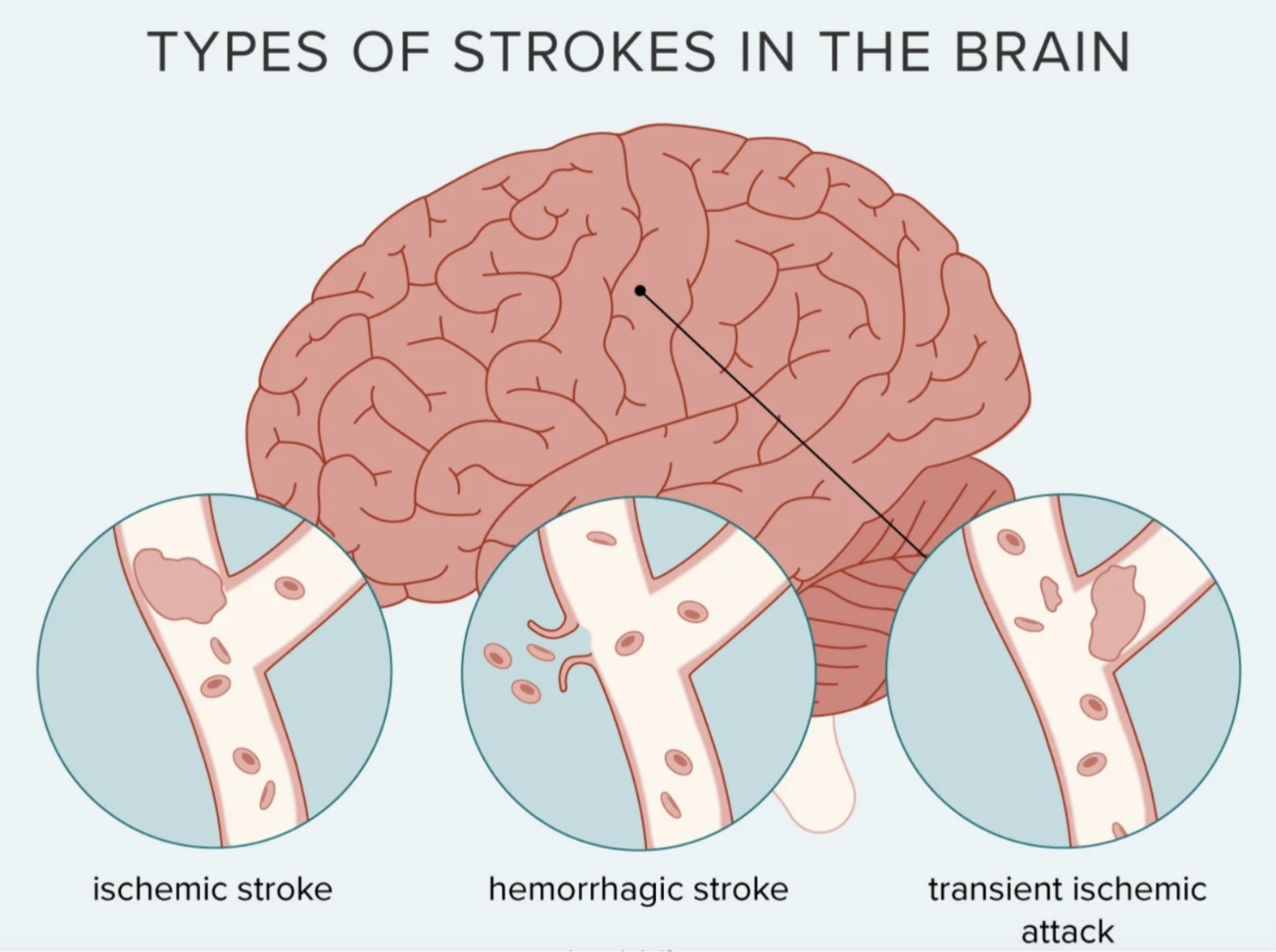
Image Source: Healthline
1. Cerebral Stroke
Cerebral strokes occur in the brain’s hemispheres, which are divided into four main lobes. Damage to these areas can result in varying symptoms, depending on the location.
• Frontal Lobe Stroke: Symptoms may include paralysis on one side, speech difficulties (such as Broca’s aphasia), personality changes, and difficulty with executive functions like planning and problem-solving.
• Parietal Lobe Stroke: Can cause numbness or sensory deficits, difficulty with spatial awareness, and neglect syndrome (especially when the right parietal lobe is affected).
• Temporal Lobe Stroke: May lead to memory problems, difficulty understanding language, and auditory hallucinations.
• Occipital Lobe Stroke: Causes visual disturbances such as difficulty recognizing faces or objects.
2. Brainstem Stroke
The brainstem is responsible for regulating essential life functions such as breathing, heartbeat, and motor control. A stroke in this area can have severe effects.
• Symptoms: Dizziness, loss of coordination and balance, double vision, difficulty swallowing (dysphagia), and weakness or paralysis on one or both sides of the body. In severe cases, locked-in syndrome can occur, in which a person is fully conscious but unable to move or communicate except through eye movements.ma.
3. Cerebellar Stroke
The cerebellum controls fine motor skills, balance, and coordination. A stroke in this area can severely impact movement and coordination.
• Symptoms: Ataxia (lack of muscle coordination), dizziness, difficulty walking, and tremors. Patients may also experience nausea and vomiting.
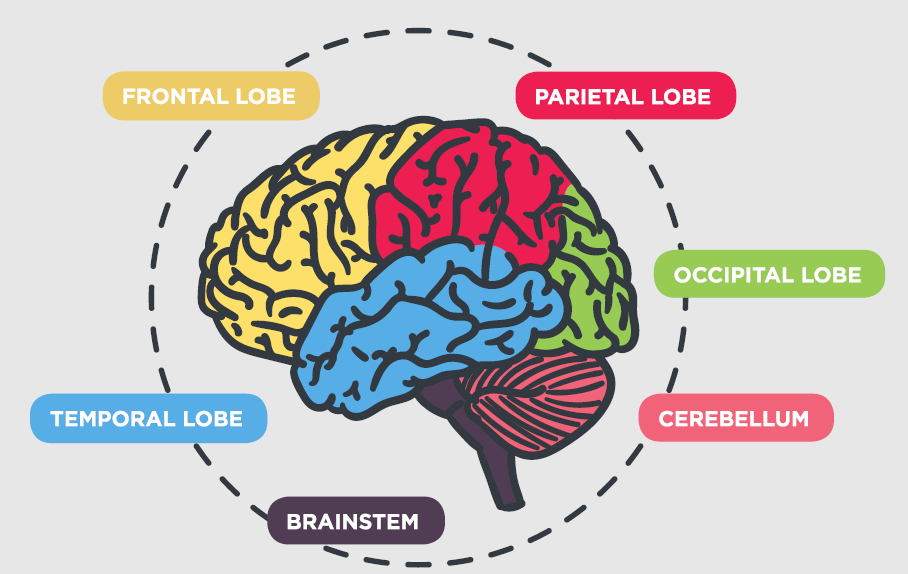
Image Source: Healthhub
• Age: Younger patients generally recover better, as their brains are more adaptable (neuroplasticity).
• Overall Health: Pre-existing conditions such as diabetes, hypertension, or heart disease can complicate stroke recovery.
• Motivation and Engagement: Active participation in rehabilitation programs, including physical therapy, speech therapy, and occupational therapy, plays a major role in improving outcomes.
• Critical Window: The first few hours after stroke onset are crucial. Immediate medical attention improves the chances of minimizing brain damage.
◦ Ischemic Stroke: The use of thrombolytic therapy (e.g., tPA) within 3 to 4.5 hours can significantly reduce brain damage.
◦ Hemorrhagic Stroke: Rapid intervention to control bleeding is critical.
• Delayed Treatment: Delays in treatment leads to extensive brain damage and poorer rehabilitation outcomes.
The type, location, affected area, and time to treatment are all critical factors that influence stroke prognosis. Early intervention, coupled with tailored rehabilitation, is essential for optimizing recovery and minimizing long-term disability. Understanding these factors helps in managing expectations and planning effective treatment strategies for stroke survivors.
If you suspect a stroke, act F.A.S.T (Face drooping, Arm weakness, Speech difficulty, Time to call emergency services) and seek immediate medical attention to increase the chances of a successful recovery.